Quick facts about melanoma skin cancer
Australia and New Zealand, have the highest rates of melanoma in the world. In Australia, melanoma skin cancer is the third most common type of cancer diagnosed
By the time you reach 85 years, you have a 1 in 13 chance of developing melanoma if you are male, and 1 in 21 if you are female
Types of melanoma skin cancer
Types of melanoma skin cancer include:
-
Superficial spreading melanoma
This is the most common type of melanoma of the skin, which often spreads from a mole as a darkish pigment under the skin.
-
Nodular melanoma
This type of melanoma often spreads downwards quickly from the outer skin layer (epidermis) to the deeper skin layer (dermis).
-
Lentigo maligna melanoma
This type of melanoma appears as a darkish irregular patch and is the least common form of melanoma.
-
Acral lentiginous melanoma
This type of melanoma appears on the soles of the feet or the palms of the hand and looks like a dark bruise.
Signs and symptoms of melanoma skin cancer
As signs and symptoms for melanoma can be similar to other common conditions, it’s important to see your GP or healthcare professional if you experience any of the symptoms below. Discussing anything concerning as soon as possible can help give you peace of mind and offer the best chance of successful treatment if you receive a melanoma diagnosis.
The first sign you may notice is a new mole or one that changes in appearance:

Size
The mole may increase in size

Colour
The colour of the mole may change and become blotchy

Evolving
The mole may bleed or itch

Height
The mole may become raised

Border
The edges of the mole may become irregular or asymmetrical
Dark patches under the nails and the lining of the mouth, vagina or anus can also be a sign of melanoma
Stages of melanoma skin cancer
Usually a biopsy will be performed to stage melanoma skin cancer, alongside other tests and investigations which help doctors understand what your cancer looks like.
This may include:
Histopathology (tissue) staging – Analysis of the cells under a microscope
Clinical staging – Clinical examination of the lymph nodes
Imaging – Body scans including CT, MRI and PET scans.
This information helps determine the stage of your melanoma using the guidelines below:
-
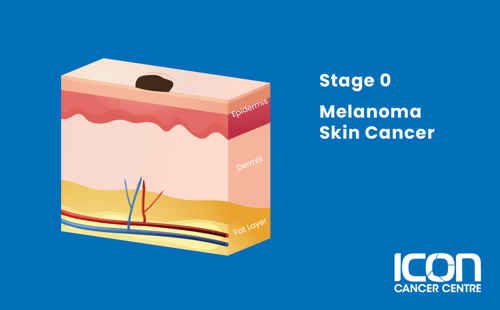
Stage 0
The depth of the melanoma is less than 0.1 mm.
-
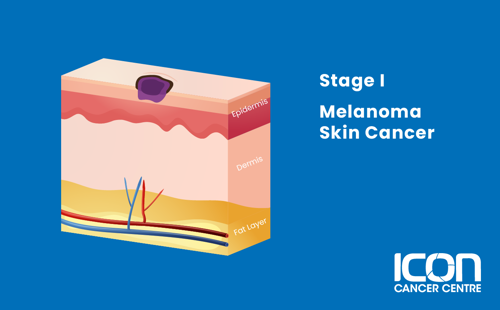
Stage I
The depth of the melanoma is less than 2 mm.
-
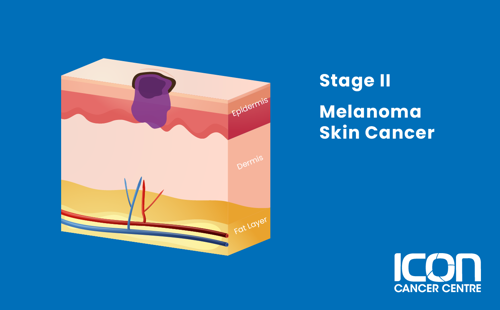
Stage II
The depth of the melanoma is greater than 2 mm.
-
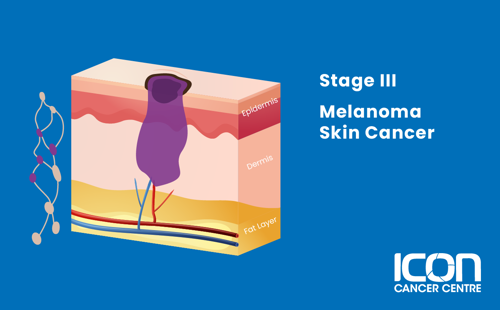
Stage III
The melanoma has spread to the lymph nodes, to very small areas of nearby skin (satellite tumours), or more than 2 cm away from the primary tumour within lymphatic vessels (in-transit metastases).
-
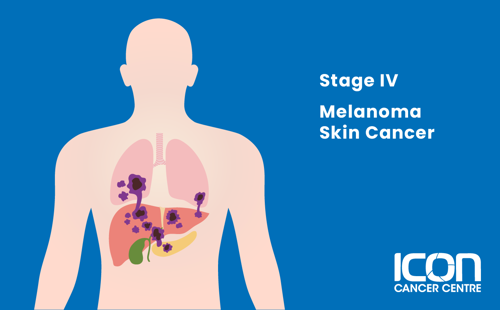
Stage IV
The melanoma has spread to distant areas of the body.
Treatment for melanoma skin cancer
There are many different types of treatment for melanoma skin cancer. Your treatment will depend on you and your cancer.




