Quick facts about uterine cancer
Uterine cancer is the most diagnosed gynaecological cancer in Australia and the fifth most common cancer in Australian women, accounting for 4.6% of all new cancer diagnoses in women
It is estimated that 1 in 44 women will be diagnosed with uterine cancer by the age of 85
Types of uterine cancer
The uterus is part of the female reproductive system and is made up of two layers: the myometrium (the outer layer of muscle tissue) and the endometrium (the inner layer or lining).
There are two main types of uterine cancer, which depend on the layer of the uterus that the cancer develops in:
-
Endometrial cancer
Cancer that develops in the endometrium. This is the most common type of uterine cancer.
-
Uterine sarcoma
Cancer that develops in the myometrium. This type of uterine cancer accounts for 2-4% of all uterine cancer diagnoses.
Signs and symptoms of uterine cancer
As signs and symptoms for uterine cancer can be similar to other common conditions, it’s important to see your GP or healthcare professional if you experience any of the symptoms below. Discussing anything concerning as soon as possible can help give you peace of mind and offer the best chance of successful treatment if you receive a uterine cancer diagnosis.
Uterine cancer can be difficult to detect as it may not cause any symptoms at early stages. As the disease progresses, symptoms can include:

Abnormal vaginal bleeding

Pelvic pain

Unexplained weight loss

Unpleasant smelling and/or watery discharge

Difficulty urinating

Pain during sexual intercourse
Stages of uterine cancer
Uterine cancer is typically staged using the FIGO (International Federation of Gynaecology and Obstetrics) system, which helps define what your cancer looks like.
Within each stage of uterine cancer, there are sub-stages listed from A through to D which describe the extent of the tumour. The FIGO system, along with other tests, helps determine the stage of your uterine cancer using the guidelines below:
-
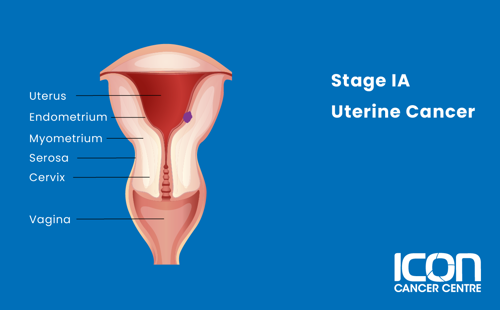
Stage IA
The tumour is confined to the inner half of the thickness of the myometrium.
-
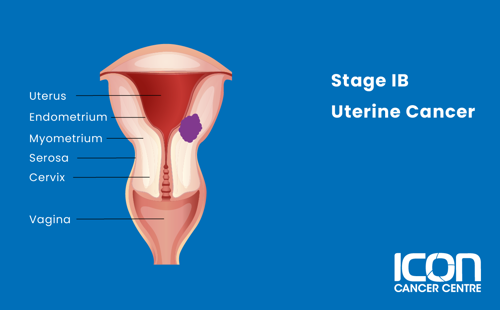
Stage IB
The tumour involves more than half of the thickness of the myometrium.
-
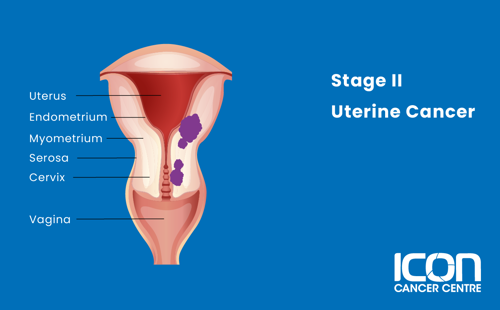
Stage II
The tumour has spread to the cervical stroma, but not outside the uterus.
-
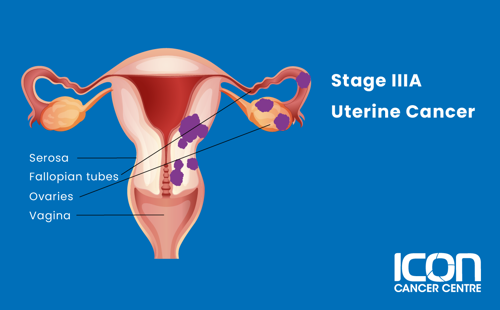
Stage IIIA
The cancer has spread to the serosa, fallopian tubes and/or ovaries.
-
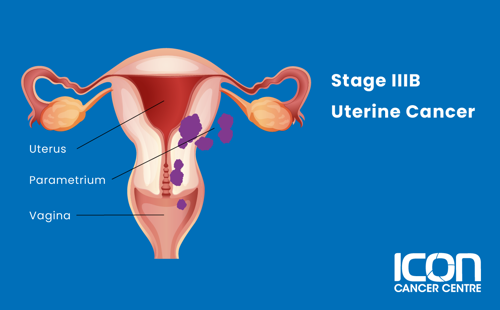
Stage IIIB
The cancer has spread to the vagina or tissue around the uterus (parametrium).
-
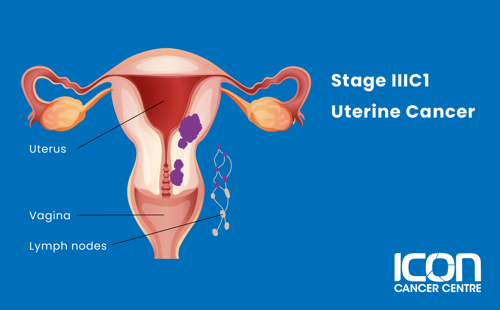
Stage IIIC1
The cancer has spread beyond the uterus to the pelvic lymph nodes, but not to the inner lining of the rectum or urinary bladder.
-
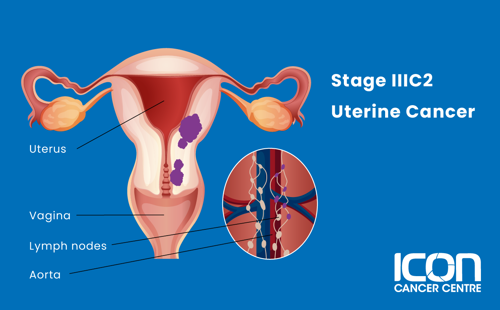
Stage IIIC2
The cancer has spread beyond the uterus to the lymph nodes around the aorta, but not to the inner lining of the rectum or urinary bladder.
-
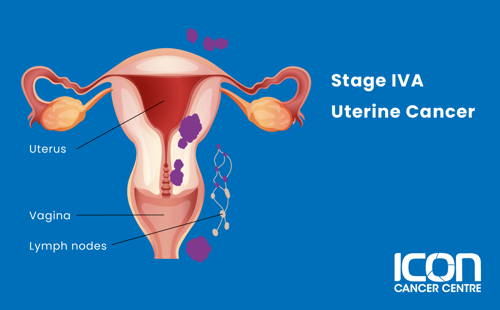
Stage IVA
The cancer has spread to the inner lining of the rectum or urinary bladder, and may or may not have spread to surrounding lymph nodes.
-
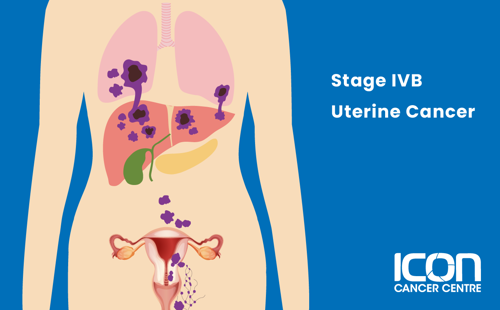
Stage IVB
The cancer has spread to the inguinal lymph nodes, the upper abdomen, omentum or distant organs including the lung, liver or bones.
Treatment for uterine cancer
There are many different types of treatment for uterine cancer. Your treatment will depend on you and your cancer.




