Quick facts about bowel cancer
Most bowel cancer starts with the development of growths, called polyps, on the inner lining of the intestine
Bowel cancer is the second most common cancer in both men and women in Australia and is more common in people over the age of 50
Types of bowel cancer
Bowel cancer refers to both colon cancer and rectal cancer.
-
Colon cancer
Colon cancer originates in the large intestine, also known as the colon. In many cases, early signs of colon cancer include non-cancerous polyps in the colon.
-
Rectal cancer
Rectal cancer develops in the end of the large intestine, known as the rectum. Like cancer found in the large intestine, it can begin with the formation of non-cancerous polyps.
Signs and symptoms of bowel cancer
As signs and symptoms for bowel cancer can be similar to other common conditions such as haemorrhoids, it’s important to see your GP or healthcare professional if you experience any of the symptoms below. Discussing anything concerning as soon as possible can help give you peace of mind and offer the best chance of successful treatment if you receive a bowel cancer diagnosis.
Symptoms may include:

Sudden changes in bowel movements, like diarrhoea, constipation, narrower stools, or stools that contain mucus

Unexplained weight loss or loss of appetite

Bright red or dark blood in your stool or on the toilet tissue

Pain in your stomach with or without swelling

Constant gas or bloating in the bowel or rectum

A lump or pain around the anus

Unexplained anaemia (low iron) which can cause tiredness and breathlessness
Download your free bowel cancer guide
Be informed, feel empowered. Our free guide will help you make decisions about your, or your loved ones, care.
Stages of bowel cancer
The TNM system is used to stage bowel cancer and define what your cancer looks like. The TNM stands for:
Tumour – The degree to which the tumour has affected other tissue, for example has it grown outside the wall of the rectum or colon
Node – Is a measure of whether lymph nodes have been affected
Metastasis – The degree to which the cancer has spread to other organs of the body
The TNM information, along with other tests, helps determine the stage of your bowel cancer using the guidelines below:
-
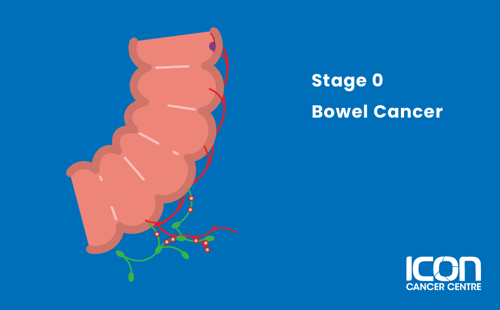
Stage 0
The cancer is in its earliest stage and has not spread beyond the inner layer (mucosa) of the colon and rectum.
-
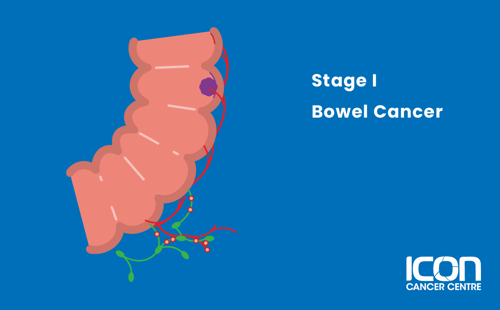
Stage I
The cancer has been found in the mucosa, and has spread beyond the inner layer of the colon or rectum to the submucosa, but not to the lymph nodes.
-
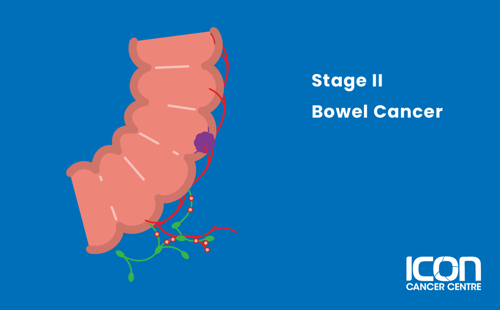
Stage II
The cancer has spread beyond the layer of muscle surrounding the bowel and reached the outermost layers of the colon or rectum and surrounding areas, but has not spread to the lymph nodes.
-
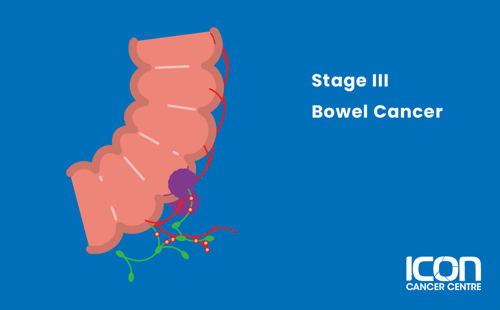
Stage III
The cancer has spread to the lymph nodes, but not to distant organs.
-
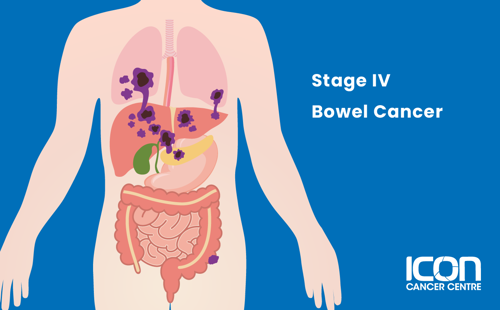
Stage IV
The cancer has spread to distant organs (e.g. lung, liver, peritoneum) throughout the body.
Treatment for bowel cancer
There are many different types of treatment for bowel cancer. Your treatment will depend on you and your cancer.




