Quick facts about anal cancer
Anal cancer is considered a rare cancer and accounts for less 500 new cancer cases diagnosed in Australia each year
Cases of anal cancer have increased over the past decade
80% of anal cancer cases are caused by the human papillomavirus (HPV).
Types of anal cancer
While most anal cancers are squamous cell cancers (SCC), they can also be classified as basal cell carcinoma (BCC), melanoma or adenocarcinoma of the anus.
Signs and symptoms of anal cancer
As signs and symptoms for anal cancer can be similar to other common conditions, it’s important to see your GP or healthcare professional if you experience any of the symptoms below. Discussing anything concerning as soon as possible can help give you peace of mind and offer the best chance of successful treatment if you receive an anal cancer diagnosis.
Symptoms of anal cancer include:

Frequent urge to defecate

Difficulty controlling bowel movements

Blood or mucus in stool

Pain, discomfort or itching around the anus
Stages of anal cancer
The TNM system is used to stage anal cancer and define what your cancer looks like. The TNM stands for:
Tumour (T) – describes the size of the tumour and the extent the cancer has spread. The tumour can be graded from T1 (describing a tumour 5cm or less) to T2 (greater than 5cm)
Nodes (N) – describes whether the tumour has spread to nearby lymph nodes. Nodes can be graded from N0, where there has been no spread, through to N1, where the cancer has spread the lymph nodes
Metastasis (M) – describes whether the cancer has spread to other areas of the body. Metastasis can be graded from M0, where there has been no spread through to M1, where the cancer has spread to other organs of the body and produced additional tumours.
The TNM information, along with other tests, helps determine the stage of your anal cancer using the guidelines below:
-
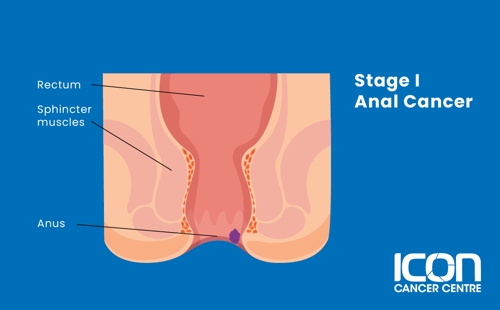
Stage I
The tumour is less than 2 cm in size
-
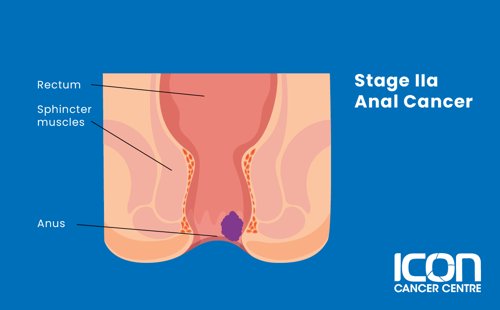
Stage IIA
The tumour is between 2 to 5 cm in size
-
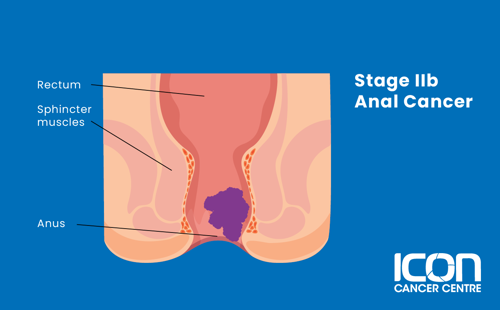
Stage IIB
The tumour is larger than 5 cm in size and has not spread to any surrounding organs or lymph nodes
-
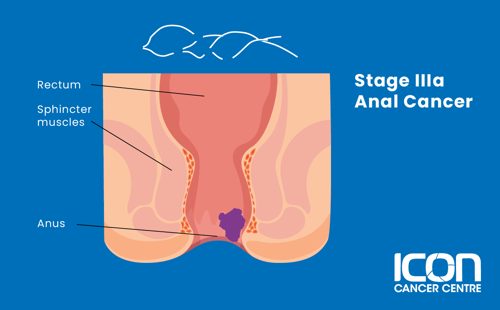
Stage IIIA
The tumour is no larger than 5 cm in size and has spread to surrounding lymph nodes
-
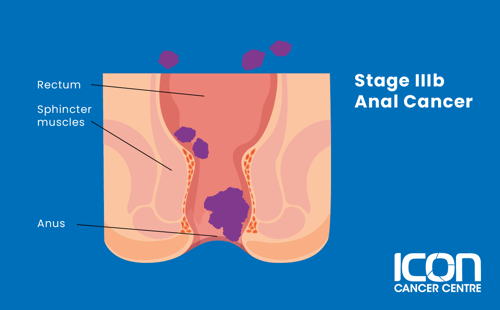
Stage IIIB
The tumour is any size and has spread to surrounding organs including the bladder, urethra or vagina, but not to the surrounding lymph nodes
-
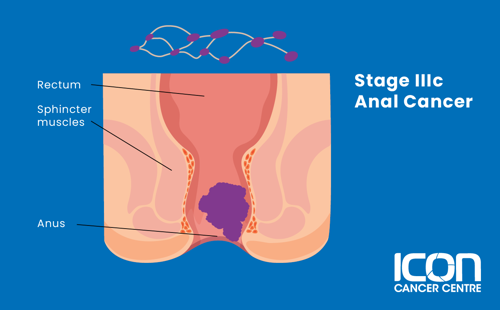
Stage IIIC
The tumour is larger than 5 cm and has spread to surrounding lymph nodes but not to other body parts. Alternatively, the tumour is any size and has spread to surrounding organs and lymph nodes
-
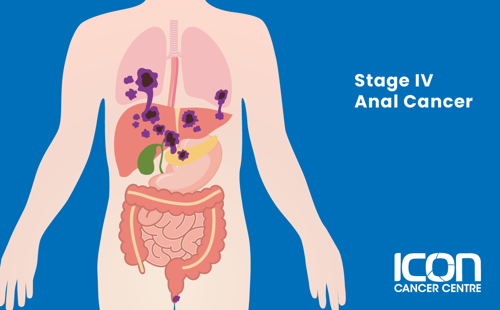
Stage IV
The cancer has spread to distant organs of the body including the liver
Treatment for anal cancer
There are many different types of treatment for anal cancer. Your treatment will depend on you and your cancer.




