What is Lutetium-177 PSMA therapy?
Lutetium-177 Prostate Specific Membrane Antigen (Lu-177 PSMA) therapy is a personalised treatment that aims to relieve symptoms and potentially slow the growth and spread of a person’s prostate cancer. It is used in the therapy phase of theranostics.
PSMA - The target
To understand how Lu-177 PSMA therapy works, it’s important to first understand what PSMA is.
Prostate Specific Membrane Antigen (PSMA) is a protein found on the surface of cells in the prostate gland. Prostate cancer cells, even those that have moved to other areas of the body (metastasised), typically have more PSMA than normal cells.
Lu-177 PSMA therapy uses this protein as a target to help identify and destroy prostate cancer cells.

The role of diagnostic imaging in Lu-177 PSMA Therapy
To determine if Lu-177 PSMA therapy is suitable for you, a PSMA PET/CT scan is used to identify if (and how much) PSMA is present on your prostate cancer cells. Click through the steps below to find out how this works.
-
Step 1
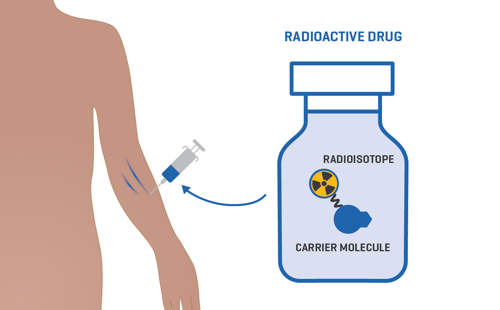
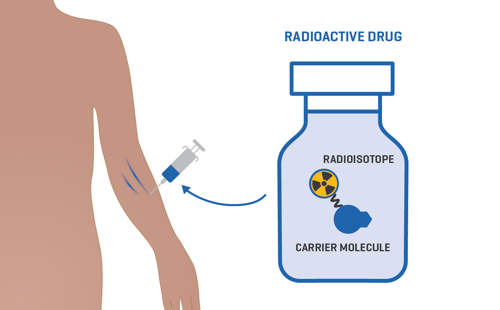
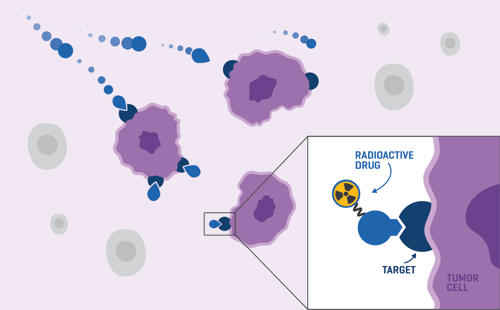
Before the PSMA PET/CT scan, a radioactive drug called a radiopharmaceutical is injected into your bloodstream. The drug is made up of a radioisotope (which gives off a small amount of radiation) connected to a carrier molecule. This carrier molecule can attach to cells with PSMA proteins on the surface (prostate cancer cells).
-
Step 2
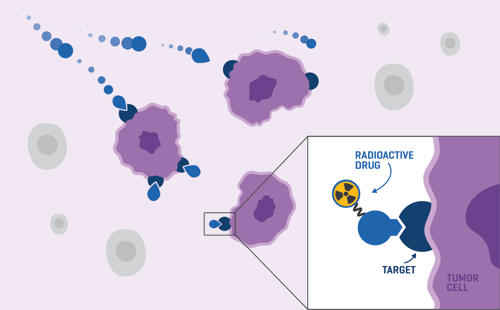
Once in your bloodstream, the drug finds and attaches to the prostate cancer cells in your body.
-
Step 3
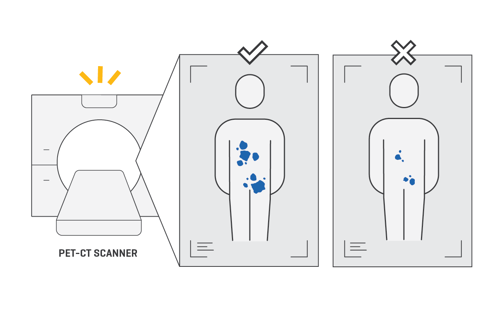
The small amount of radiation from the radioisotope then shows up as ‘hot spots’ on a PET/CT scan.
Along with other imaging scans like an MRI and CT scan, this helps your doctor understand exactly where the cancer is throughout the body (even tumours that are a few millimetres in size) and organise a personalised treatment plan for you.
How Lu-177 PSMA Therapy works
If you are determined suitable for Lu-177 PSMA therapy, you can proceed to treatment. Click through the steps below to find out more.
-
Step 1
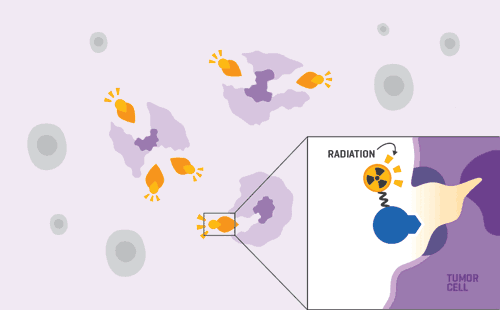
For therapy, a different radiopharmaceutical (radioactive drug) is injected into your bloodstream.
This drug also contains a molecule that can attach to cancer cells with PSMA on the surface (prostate cancer cells), however it carries a different radioactive isotope called Lutetium-177.
Lutetium-177 gives off a different type of radiation that aims to injure or kill cancer cells.
-
Step 2
Once in your bloodstream, the drug finds and attaches to the prostate cancer cells in your body. This carries the radioactive Lutetium-177 directly to the cancer cells.
-
Step 3
Once attached, the radiation released from the radioisotope injures and potentially kills the cancer cells without damaging the healthy cells around them.
We're here for you, every step of the way.
To learn more about Lu-177 PSMA Therapy or find out where to receive this treatment at Icon, go back to our theranostics page.




