Quick facts about lung cancer
About 11 in 500 Australians develop lung cancer each year
Lung cancer is the fifth most common cancer type
Lung cancer is the leading cause of cancer death in Australia
Types of lung cancer
Lung cancer is either classified as non-small cell lung cancer (NSCLC) or small cell lung cancer (SCLC).
-
Non-small cell lung cancer (NSCLC)
This is the most common form of lung cancer, making up 85% of all lung cancer cases. NSCLC can be classified into:
Adenocarcinoma – Typically found on the outer area of the lungs, in cells that produce mucus
Squamous cell carcinoma – Typically found in the airways of the lungs
Large cell undifferentiated carcinoma – This type of cancer can not be classified as either adenocarcinoma or squamous cell carcinoma, and is therefore grouped into its own subcategory.
-
Small cell lung cancer (SCLC)
This type of lung cancer tends to spread faster than NSCLC. SCLC is less common than NSCLC, accounting for 15% of all lung cancers.
Signs and symptoms of lung cancer
As signs and symptoms for lung cancer can be similar to other common conditions, it’s important to see your GP or healthcare professional if you experience any of the symptoms below. Discussing anything concerning as soon as possible can help give you peace of mind and offer the best chance of successful treatment if you receive a lung cancer diagnosis.
Symptoms may include:

Wheezing, coughing or difficulty breathing

Difficulty swallowing

Coughing up blood

Unexplained tiredness or fatigue

Swollen face or enlarged veins in the neck

A chronic (ongoing) cough that doesn’t go away

Shoulder or chest pain that may be worse with breathing

Chronic infections such as bronchitis or pneumonia
Download your free Lung Cancer Treatment Guide
Be informed, feel empowered. Our free guide will help you make decisions about your, or your loved ones, care.
Stages of lung cancer
The TNM system is used to stage lung cancer and define what your cancer looks like. The TNM stands for:
Tumour (T) – Describes the size of the tumour and the extent the cancer has spread into the tissue of the lung. The tumour can be graded from T1a (which describes a tumour under 1 cm) to T4 (which describes a tumour larger than 7 cm)
Nodes (N) – Describes whether the tumour has spread to nearby lymph nodes. Nodes can be graded from N0, where there has been no spread, through to N3, where the cancer has spread to other areas of the body, such as the other side of the chest or collarbone
Metastasis (M) – Describes whether the cancer has spread to other areas of the body outside of the lung. Metastasis can be graded from M0, where there has been no spread through to M1c, where the cancer has spread to other organs of the body and produced additional tumours.
The TNM information, along with other tests, helps determine the stage of your lung cancer using the guidelines below:
-
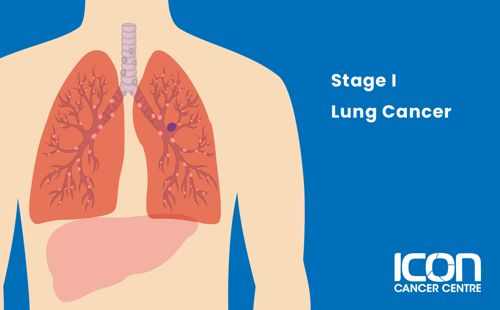
Stage I
The tumour is 5 cm or less across, affects the main branches of the bronchi and has not spread beyond the lungs.
-
Stage II
The tumour is 7 cm or less across and has spread to nearby lymph nodes. Alternatively, there may be one separate tumour nodule present.

-
Stage III
The tumour can be any size and has spread to the lymph nodes. It may have also spread to surrounding areas. Two or more separate tumours are present in different lobes of the same lung.

-
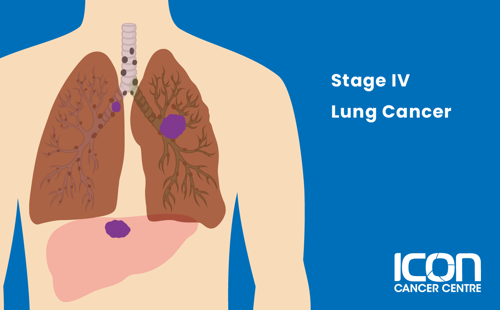
Stage IV
The tumour in the lung can be any size and has spread to distant organs within the body.
Treatment for lung cancer
There are many different types of treatment for lung cancer. Your treatment will depend on you and your cancer.




